
Did you know that you probably have helicobacter pylori in your stomach? A lot of people do. Most of the time, this bacteria (also known as H. pylori) is harmless. “Bacteria” doesn’t have to be a bad thing – there are good and not-so-good bacteria in your stomach all the time. Is h. pylori good or not-so-good? While the presence of this bacteria is common, h. pylori can cause ulcers, inflammation, and even stomach cancer.
Monitoring the h. pylori in your stomach, understanding how diet affects h. pylori, and staying on top of the presence of stomach ulcers can help prevent inflammation and more serious complications.
What Is H. Pylori?
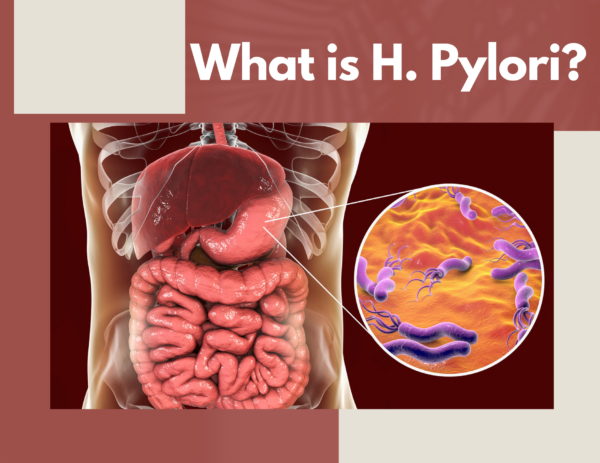
H. pylori is a bacteria that grows in and affects the stomach. This spiral-shaped bacteria, while potentially harmless, may cause ulcers and inflammation. Not much is known about the contraction of h. pylori, but it exists in close to half the population.
Different parts of the h. pylori bacteria help it navigate the stomach (and potentially cause damage.) Dangling from its spiral-shaped structure are flagella that allow it to move around. Around the structure are lipopolysaccharides that attach the bacteria to stomach cells. Also around the structure is the enzyme urease, which converts urea in the stomach to carbon dioxide and ammonia. Urease is the reason that h. pylori can survive the extremely acidic environment of the stomach, while many other types of bacteria can’t.
Problems occur when the carbon dioxide and ammonia neutralize stomach acid. Stomach acid is key to breaking down food, absorbing nutrients, and easing digestion. A layer of stomach acid also protects bacteria from stomach cells. When h. pylori neutralizes stomach acid, they can access and adhere to stomach cells. Once attached to stomach cells, h. pylori bacteria secretes exotoxins that can cause peptic and duodenal ulcers and disrupt cell integrity.
H. Pylori vs Ulcers

For years, scientists believed that stress and spicy foods were the cause of ulcers, or painful sores in the stomach lining. When h. pylori was identified as the real catalyst, researchers were met with doubt. There are still a lot of questions as to why around one in ten people experience stomach ulcers when up to half of the population has h. pylori in their stomachs. What we do know is that the presence of exotoxins cagA and vacA, made by h. pylori, are associated with a higher risk of ulcers in the stomach and small intestine.
H. Pylori vs E. Coli
H. pylori and e. coli are both types of bacteria that live in the digestive system. H. pylori is more likely to be found in the stomach, while e. coli lives in the intestines. Both bacteria have the potential to be harmless. When they do cause harm, however, they cause very different types of harm. E. coli can cause symptoms that include UTIs, diarrhea, vomiting, and cramps. You cannot get an ulcer just because your intestines contain e. coli.
Both forms of bacteria can be spread from hand-to-mouth contact, but e. coli is typically spread through the consumption of contaminated food and water. Researchers are still not sure exactly how H. pylori is spread, although they do believe it is through hand-to-mouth contact and may be contracted if consuming contaminated food and water.
H. Pylori vs SIBO

SIBO, or Small Intestine Bacterial Overgrowth, is a condition caused by too much, or the wrong types of, bacteria in the small intestine. Often, bacteria meant to be in the large intestine may be present in the small intestine, leading to various complications.
The good news is, breath tests can help you determine whether your symptoms are caused by h. pylori, SIBO, or the presence of other types of bacteria. I use the following tests to check on the health of my digestive system:
Small Intestinal Bacterial Overgrowth 2-Hr Lactulose (SIBO, BOSI)-Genova Kit
H. Pylori vs Norovirus
Norovirus is a virus and h. pylori is a bacteria. Bacteria, unlike viruses, are living organisms. This key difference doesn’t change the fact that bacteria and viral infections often have the same symptoms. Norovirus can cause gastroenteritis, or the common stomach virus. Like the e. Coli bacteria, diarrhea, vomiting, and cramps may be a sign of gastroenteritis.
Studies are still being done to understand the link between h. pylori and gastroenteritis, although some have revealed that h. pylori does not cause gastroenteritis, but h. pylori infections may be transmitted in the same way that the stomach virus is transmitted.
H. Pylori was only discovered in the 1980s – there is still so much that the public and even researchers do not know about this bacteria. In this series, I will share what is known about H. Pylori and how you can treat h. pylori and prevent the complications that may be caused by h. pylori. One of the most effective ways to treat h. Pylori is actually quite simple! One cup of matula tea in the morning and one at night (on an empty stomach) can eliminate h. Pylori and reverse the damage that this bacteria can cause.
Have you heard of h. pylori before this blog post? Has your healthcare provider mentioned it while discussing stomach complications? Let us know below.
***You can buy Matula Tea here.***

Latest posts by Sylvie McCracken (see all)
- Treating H. Pylori (Part 3): What H. Pylori Does to the Body - August 8, 2022
- Treating H. Pylori (Part 2): How H. Pylori is Contracted - August 3, 2022
- Understanding Beef Labels: Organic, Pastured, Grass-Fed & Grain-Finished - July 25, 2022