Do you have a gut condition like SIBO, IBS, or IBD? The first step to curing gut problems is to learn how your digestive system works. This brief guide will go over the esssential steps in digestive — including those that most articles gloss over — so you can start to understand the real underlying problems causing your gut condition.
What Controls Digestion?
There are three main things which control the digestion process:
- Hormone Regulators (Endrocrine System): There are cells lining the stomach and small intestine. These cells release hormones which help control digestion, such as by stimulating the production of gastric juices.
- Extrinsic Nerves (Central Nervous System): Extrinsic means “external” and refers to the nerves which connect the digestive organs to the spinal cord and brain. These are stimulated by touching, tasting, or thinking about food.
- Intrinsic Nerves (Enteric Nervous System): These are the nerves which are within the GI tract and are part of their own nervous system called the Enteric Nervous system, or ENS. They are triggered when food touches them. Once stimulated by food, they trigger the production of gastric juices and also regulate how quickly food moves throughout the GI tract.
(Source 1)
Sadly, most people don’t talk much (or at all) about the role of hormones and nerve signals in digestion. Instead, they mostly focus on gastric juices. Sorry people, but it is actually hormones and the nervous system which are controlling gastric juices! And what controls hormones and nerve signals? Some of this is controlled by the brain, which is why stress can cause indigestion. But researchers now know that much of digestion (and many other bodily functions) are controlled by the bacteria residing in our guts. An imbalance in gut bacteria is the likely cause of gut diseases including SIBO, IBS, IBD, ulcers, and acid reflux.
Pre-Food Stage of Digestion
We think of digestion as something which happens when we eat food but digestion can begin even before food enters our mouth. When we smell or see food, or even just think about food, it causes the cerebral cortex to light up. The stimulus travels to your hypothalamus then to the brain stem, and down the vagus nerve. The vagus nerve connects to every organ in the body except the adrenal glands. Yes, EVERY organ except the adrenals. The vagus nerve tells the stomach to start churning in preparation for food (which is one reason why your stomach rumbles when you are hungry and see food) and gets our saliva going. Gastric juices also start to increase. This entire “pre food” stage of digestion is called the cephalic or neural phase.
The Esophagus
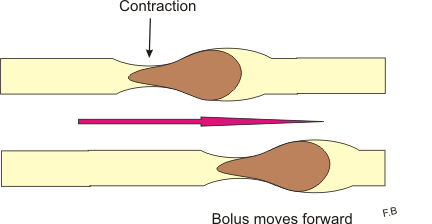
Once you actually consume some food, the gastric phase of digestion begins. This is where things really get going. Your saliva starts breaking down starches. You swallow and the chewed food (which is called bolus) travels to the esophagus. A series of strong, wave-length contractions push the bolus into the stomach. These contractions are called peristalsis and peristalsis waves continue into the stomach and through the intestines. It is important to note that peristalsis is controlled by the enteric nervous system. If your enteric nervous system isn’t working properly, then persistalsis can malfunction too. More on this later.
The Stomach
When bolus enters the stomach, it touches the nerves inside the stomach and tells them to release more gastric juices. Peristalsis waves churn the bolus with the gastric juices. These juices, along with many acids, start breaking down food into molecules that can be absorbed by the body. Once the food is broken down, it turns into a substance called chyme.
The chyme goes through a “gateway” called the pyloric valve. This valve allows chyme from the stomach to enter the duodenum, which is the start of the small intestine. Only a little bit of chyme is allowed through at once. The rest is stored in the stomach until the small intestine is ready for it. This is important because the body needs time to absorb the nutrients in the food you eat. If all of the food from the stomach entered the small intestine quickly, the small intestine wouldn’t be able to absorb the nutrients efficiently. It takes about 3-4 hours for a typical meal to completely leave the stomach. However, some foods can stay in the stomach for a much shorter or longer time.

The pyloric valve can also open when the stomach is empty. This happens as part of a type of motility called the migrating motor complex (MMC). Unlike persistalsis in which the purpose is to move food, the MMC acts as a “housekeeper.” It is triggered only when the stomach is empty and its contractions clean out any remaining particles from the stomach and intestines. The MMC is a function of the nervous system (you’ll note a common theme here that digestion is a nervous system function!). If the MMC isn’t working properly, you can end up with undigested food particles stuck in your stomach and waste in your intestines. These waste products can damage your digestive tract and cause a buildup of “bad” bacteria. This disrupts your gut flora and can lead to gut problems. (Source 1)
The Small Intestine
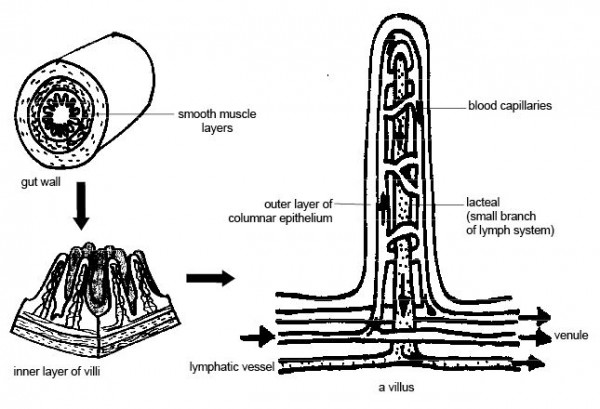
The small intestine, which is on average 20 feet long, is arguably the most important part of the digestion process. It is in the small intestine that chyme is broken down into absorbable nutrients. The small intestine is responsible for getting these nutrients into our bloodstreams so we can use them. The first few inches of the small intestine are smooth, but the remaining are made up of many folds called mucosal folds. There are also finger-like projections called villi lining the small intestine. The villi increase the surface area of the small intestine and help absorb more nutrients, much like how a towel’s textured fabric help it absorb more water.
To break down chyme, the liver releases bile which emulsify fats. The pancreas releases pancreatic juices which break down fatty acids and also break down carbohydrates and proteins. After several hours of digestion, the food you ate is broken down into its smallest compounds and they are ready to be absorbed into your bloodstream. Bacteria in the small intestine also produce some enzymes which are needed to break down carbohydrates.
After the small intestine has done its job of absorbing nutrients (assuming that it is working properly), the remaining waste is pushed into the large intestine. The large intestine absorbs liquid from the waste, turning it into stool. The rectum will store the stool until it is pushed out during a bowel movement.
If the small intestine is damaged, then it won’t be able to absorb nutrients effectively. The result can be severe nutrient deficiencies. Since bacteria in the gut is also in charge of producing certain nutrients (like vitamin K), a disruption in your gut flora can also lead to deficiencies. These deficiencies can go on to cause numerous other health problems — like how people with IBD often have night blindness as a symptom due to the nutrient deficiencies they develop. (Source 1, 2, 3)
Large Intestine
By the time chyme leaves the small intestine (assuming it is working properly), there are hardly any nutrients left in it. It is no longer called chyme but considered to be fecal matter. The large intestine’s main role is to reabsorb the water from the waste so it can be reused by the body. However, it also absorbs some nutrients and has a role in producing antibodies. There are 4 separate parts of the colon and each has a different role in digestion:
Cecum
This is the first part of the large intestine. It is connected to the small intestine through the ileocecal valve. When the cecum becomes distended, it triggers the ileocecal valve to close, thus preventing the backflow of fecal matter into the small intestine. If the ileocecal valve is malfunctioning, then you could get fecal bacteria in your small intestine, causing bacterial overgrowth, aka SIBO. (Source)
Ascending, Transverse, and Descending Colon
When fecal matter arrives in the ascending colon, it is still a liquid. The main role of the ascending colon is to absorb this liquid. About 5 gallons of fluids are dumped in the large intestine each day. Contractions push it further along to the transverse and then descending colon. As the fecal matter moves throughout the colon, more and more water is absorbed from it. By the time that fecal matter arrives at the descending colon, it is no longer liquid but a semi-solid.
If the large intestine didn’t reabsorb these fluids, the body would get dehydrated quickly. A series of mostly un-rhythmic contractions in the large intestine mix waste back and forth without pushing it forward. These contractions help the large intestine absorb more fluids. However, it also takes a long time to reabsorb the water. Waste remains in the large intestine for about 30 hours before it is passed out as a bowel movement. (Source 1, 2)
Again, remember that gut contractions are regulated by the nervous system. If your nervous system isn’t causing the gut to contract properly, you can end up with too little water absorbed (diarrhea) or too much water absorbed (constipation).
Loperamide, the anti-diarrheal medicine which is often prescribed for diarrhea, works by acting on the receptors of the large intestine so waste stays in the large intestine longer, thus allowing more fluids to be absorbed. It does not solve the underlying cause of the problem which is that your bowels aren’t contracting properly.
Fiber in food we eat is what causes stool to be soft so it passes easier. Taking fiber for constipation can make passing stool easier. But this too does not solve the underlying problem that the bowel isn’t contracting properly.
The Sigmoid Colon
The sigmoid colon is the last stop before fecal matter goes to the rectum and is pushed out in a bowel movement. For most IBS patients, the sigmoid colon is the major source of pain. One reason for the pain is because stools become solid here. Another reason for the pain is because the sigmoid colon has notably stronger contractions than the rest of the colon. These contractions are necessary to push fecal matter into the rectum. In patients with IBS, the contractions are very chaotic and frequent compared to healthy controls. (Source 1, 2)
It is also possible that IBS patients have increased nerve sensitivity in their sigmoid colon. In a well-known experiment, patients with IBS had balloons inflated in their sigmoid colon. The IBS patients experienced pain at a much lower threshold than the healthy controls. The sigmoid colon might have more dispatches of pain signals to their brain. The sigmoid colon can also cause upper abdominal pain when it contracts and pushes gas up into the transverse colon. (Source)
Do you have IBS? Download our free guide 7 Things You Wish Your Doctor Told You About IBS.
Latest posts by Sylvie McCracken (see all)
- Treating H. Pylori (Part 3): What H. Pylori Does to the Body - August 8, 2022
- Treating H. Pylori (Part 2): How H. Pylori is Contracted - August 3, 2022
- Understanding Beef Labels: Organic, Pastured, Grass-Fed & Grain-Finished - July 25, 2022

Thank you for your insight. I would love to hear a NEW idea about, idiopathic gastroparesis. Mayo and other don’t seem to think we will ever get over it, due to the fact many don’t. I will! I will sit hear and research, and try everything and anything to get my health and life back, and hopefully, help others. The thing that interests me the most is that, it’s mostly young women and menopausal women who get this.Gee what do they have incommon, imbalanced hormones. I am in perimenopause, and am getting BIHRT.To see if it helps.I am already doing ALLLLLL the right things and have seen a big improvement, in 4 years, but now have it a wall….just thought you may have a novel idea? Thanks for your time and ideas, Ava PS.Don’t ever get this disease it changes you to the point it’s hard to keep going and yet you don’t have a choice.